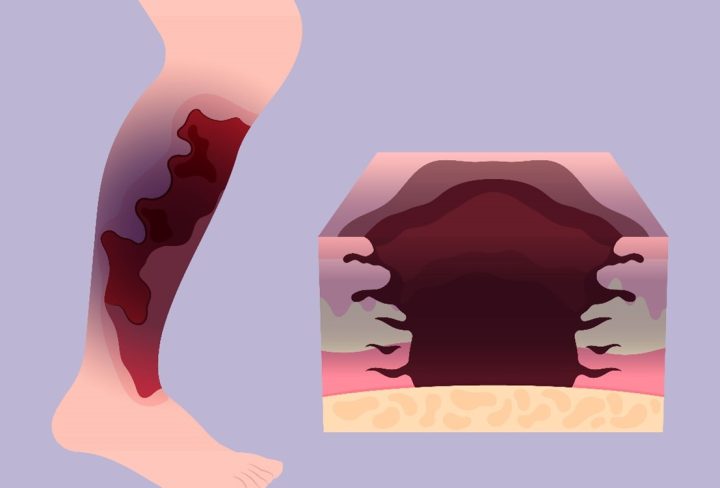
It is characterized by rapid and aggressive tissue destruction caused by bacterial infection, often involving deep layers of skin, muscle, and fascia. It progresses swiftly and can lead to systemic complications and even death if not treated promptly and effectively.
The Role of Plastic Surgery
Debridement and Tissue Removal
- Extensive Debridement: Plastic surgeons are trained to meticulously remove necrotic tissue, which is vital for halting the spread of infection and preventing further tissue damage.
- Precise Identification: They identify and remove affected tissue layers, encompassing skin, muscle, and fascia, to thoroughly eradicate the source of infection.
Soft Tissue Reconstruction
- Skin Grafts: Using skin from unaffected areas of the body (autografts) or donor sources (allografts) to cover wounds and facilitate healing.
- Local Flaps: Transferring nearby healthy tissue to cover exposed areas and aid in wound closure.
- Microvascular Free Tissue Transfer: Transplanting healthy tissue with its blood supply from distant sites to reconstruct extensive tissue loss.
Wound Management
- Advanced Techniques: Utilizing negative pressure wound therapy (NPWT) to promote healing by applying controlled suction to the wound area.
- Regular Monitoring: Ensuring timely dressing changes and ongoing wound care to maintain a clean environment and prevent recurrence of infection.
Functional and Aesthetic Restoration
- Preserving Function: Prioritizing the restoration of functional abilities, such as mobility and range of motion, through reconstructive efforts.
- Aesthetic Considerations: Addressing cosmetic outcomes by reconstructing the affected area to minimize scarring and restore a natural appearance.
Multidisciplinary Collaboration
- Team Approach: Working closely with infectious disease specialists, intensivists, and other healthcare professionals to optimize treatment outcomes.
- Comprehensive Care: Developing individualized care plans that encompass immediate surgical needs and long-term rehabilitation goals.
Long-term Monitoring and Rehabilitation
- Postoperative Care: Monitoring patients closely post-surgery to manage complications and ensure optimal healing.
- Rehabilitation Programs: Initiating physical therapy and occupational therapy to regain strength, mobility, and function during recovery.
Patient Education and Support
Patient education includes providing information on wound care, potential complications, and preventive strategies. Emotional support is also offered to help patients manage the physical and emotional challenges of surgery, ensuring comprehensive care and improved recovery outcomes.
Research and Innovation
- Advancing Techniques: Contributing to ongoing research to improve surgical techniques, wound care strategies, and outcomes for patients with necrotizing fasciitis.
- Innovative Approaches: Exploring new technologies and treatments to enhance the efficacy and safety of reconstructive procedures.
Plastic surgery for necrotizing fasciitis involves advanced surgical techniques, meticulous wound care, and comprehensive rehabilitation efforts. By integrating these components into a cohesive treatment plan, plastic surgeons play a pivotal role in not only saving lives but also restoring the function and quality of life for individuals affected by this challenging condition. Their expertise and dedication contribute significantly to improving outcomes and advancing the field of reconstructive surgery in critical care settings.